Four of ACM’s 2022 workers’ compensation claims initiatives will significantly help resolve claims more quickly, providing injured employees the latest in quality medical care and returning them to gainful employment. At the same time, they will help in lowering payouts and reducing litigation costs for employers and insurers. These four include Rebound (return-to-work), RapidResponse, Head Injury Program and Harvard Med Tech’s pilot program for virtual reality pain management therapy. Today we’ll discuss the first two.
Rebound return-to-work program
Rebound, our return-to-work program, makes the road to recovery easier for the injured worker. As the first of our workers’ compensation claims initiatives, it includes three assessment phases:
- Early return-to-work. The return-to-work nurse coordinator collaborates with treating provider to facilitate safe and appropriate work restrictions according to the official disability guidelines.
- Transitional return-to-work. The nurse coordinator manages an on-site job analysis to assist the employer in developing a modified duty accommodation. If that’s not possible, the worker is referred to an alternative duty assignment through a non-profit agency.
- Maximum medical improvement with permanent restrictions. The nurse coordinator assists the worker in creating their resume or recommends a job site analysis to help employer develop an alternative permanent position.
Rebound enables injured workers to be productive during their rehabilitation and maintain a connection with their workplace. The program works with the patient and their healthcare provider to help the injured person return to the workplace as soon as they’re medically and safely capable.
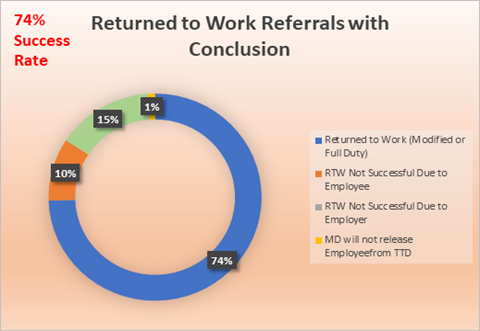
“We’ve experienced a 74 percent success rate in turning employees to work, both modified or full-duty,” explained Cheryl Gulasa, vice president of managed care. “And in 2021, we saw a total savings of $877,797 in medical claims with Rebound.”
Rebound case study
An injured employee was given work restrictions after a work-related injury. The employer did not have a modified duty program to offer, so the employee was not able to return to work.
Our nurse coordinator organized a Job Fit Analysis: an onsite job evaluation with the employer to clarify the injured worker’s job tasks and physical demands for the position. Together they documented competencies required for a job, and provided the list to the treating physician. The nurse and a representative assisted the employer in creating a modified position for the employee so that he could return to work while following the provider’s prescribed work restrictions.
The revised job resulted from the RTW coordinator’s interventions. Once work restrictions were released by the physician, the worker returned to full duty with the employer.
Related: Five pillars of a successful return-to-work program
RapidResponse
The second of our workers’ compensation claims initiatives is RapidResponse Program, a nurse triage program that focuses on historically high-cost claims for badly injured claimants. This program adds a nurse to the claim from the outset, from first report of injury. It focuses on claims that are:
- Reported 30+ days after the injury
- Continuous trauma from repetitive motion
- Complex orthopedic injuries
- Motor vehicle accidents
- Catastrophic/complex trauma
- Patients that are admitted to a hospital
- Penetrating, blunt force or rupture injuries
- Head injuries
- Traumatic events or PTSD claims
- Patient is over 65 years old
We’ve found that when the nurse establishes rapport with the injured worker, taking the time to listen to their fears and complaints, answering their questions, educating plus advocating for them, both the worker and the employer have a better grasp of the issues at hand. This leads to reduced litigation and reduced costs.
RapidResponse case study
An employee was injured on the job and tried to work through the pain, hoping it would improve on its own. In early March, he was sent to the ER by his employer because he was unable to walk. When the first report of injury was addressed by a RapidResponse nurse, the employer was concerned about how long the worker had to wait for an appointment (because he lives in a rural area). Our RapidResponse nurse pulled strings to move the claim forward quickly by communicating a revised plan with employer, educating the employee on the workers’ compensation claim process and especially by accelerating appointment scheduling using our Medical Provider Network resources. Otherwise, the employee would’ve waited a week just for an initial medical visit. Thanks to RapidResponse intervention, he had a next-day appointment.
Related: Why it pays to report work comp claims promptly
Our recent success rates of the Rebound and RapidResponse programs combined
“In 2020, our case managers were able to close just two-thirds of their files. Then, in 2021, carrier Everest implemented these two programs, and the case managers were able to wrap up 99% of the files by year-end. Once we put these components of a medical coordination program together, the end result is we are able to resolve claims significantly faster,” Gulasa explained.
Next we’ll publish the remaining workers’ compensation claims initiatives that we’re focused on in 2022, to help resolve claims faster, thereby reducing claims payouts and litigation. View the article here.